Interstitial lung disease or ILD was the shocking diagnosis Joe Crossmon received when he was hospitalized in Columbus, Ohio, in 2018. A condition more commonly seen in older patients, Joe was 35 years old at the time.
“The doctor told Joe, ‘Just come back in one year,’” recalls Paige, Joe’s wife. “He told him if it gets bad, we’ll just get you a new set of lungs. He meant it as a joke. I don’t think he suspected that was going to happen.”
Four years later, in spring 2022, Joe mowed his grass for the first time that season and became severely winded. “I remember thinking I’d really gotten out of shape over the winter,” says Joe, who had generally been in good health.

At one point, Joe needed 10 or more liters of oxygen a day. (Courtesy: Cleveland Clinic)
A month later, following a short mountain hike while visiting family in Phoenix, Arizona, Joe was again unable to catch his breath. Back home in Ashland, Ohio, he and Paige – pregnant with their third child – visited two emergency departments, as Joe’s condition worsened. He was admitted to his local hospital for five days and still struggled to breathe, barely able to hold a conversation.
That’s when Paige made an appointment for Joe to visit Cleveland Clinic’s Respiratory Institute. The pulmonologists who examined Joe immediately recognized the severity of his condition. They began a course of steroids and other immunosuppressant medications in hopes of reversing his ILD.

Joe undergoing a breathing test at Cleveland Clinic. (Courtesy: Cleveland Clinic)
But nothing worked. While Joe was able to return home after 10 days at Cleveland Clinic, and briefly resumed work at the tattoo parlor he has operated for nearly two decades, he soon required more oxygen, around the clock. Tethered to an oxygen concentrator, he needed four, then eight, and finally 10 or more liters of oxygen every day. It was a struggle to walk outside and push his pre-school-aged kids on a swing.
“Oxygen was helpful, and fortunately all my other organs were healthy and strong,” says Joe. “But for the amount I needed, I couldn’t go anywhere for very long without having two or three big tanks with me.” Adds Paige, “At that point, we still had this hope he would get better from the medications.”
According to pulmonologist Marie Budev, DO, medical director of Cleveland Clinic’s lung transplant and heart-lung transplant program, “The typical patient with ILD has stability regarding their symptoms and lung function for many years and then experiences a gradual decline. That’s not uncommon, but in a limited number of cases, such as Joe’s, the decline in lung function and respiratory status can be rapid without prior warning.”
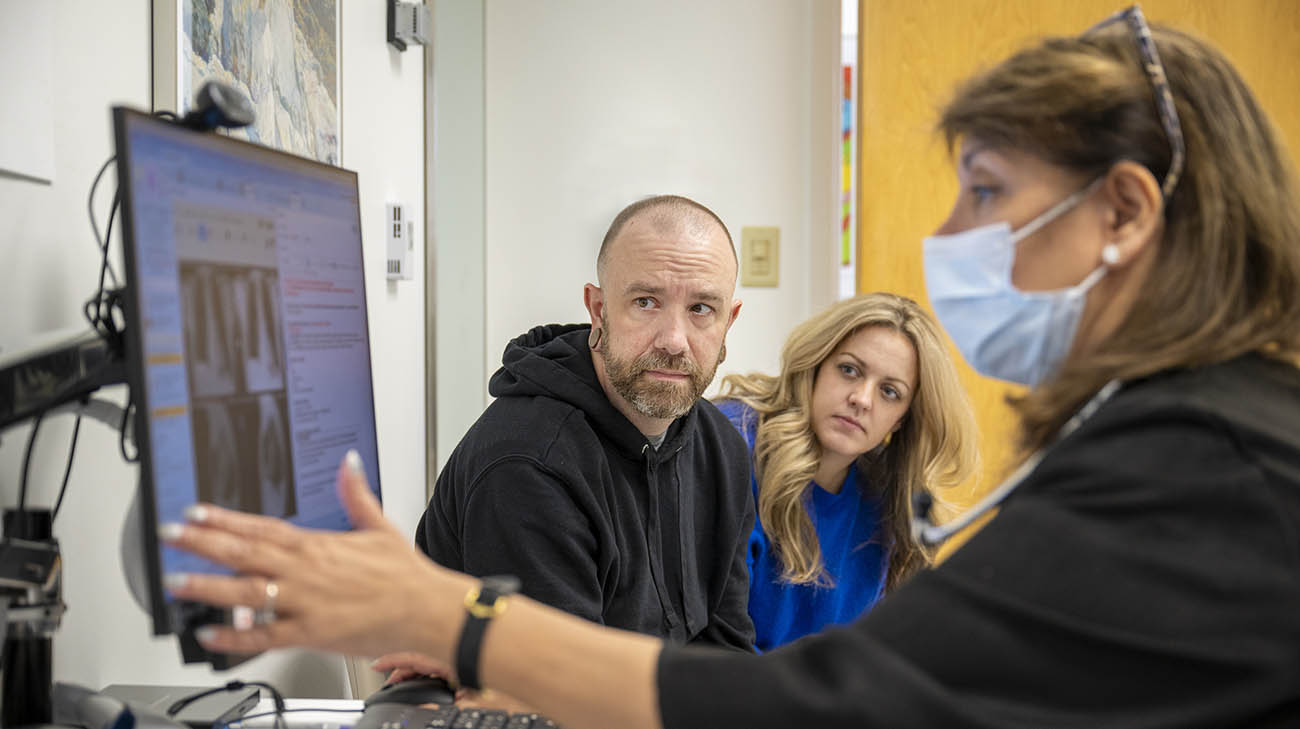
Joe and Paige during a follow-up appointment with Dr. Budev, after Joe underwent a double-lung transplant. (Courtesy: Cleveland Clinic)
On August 21, 2022, Joe was admitted again to Cleveland Clinic. At that point, his physicians began to plan for lung transplantation.
“We consider a transplant to be the last option for patients with ILD who have not responded to medical therapy. We always try to preserve their native lungs, if at all possible” says cardiothoracic surgeon Kenneth McCurry, MD, who consulted on Joe’s case as surgical director of Cleveland Clinic’s lung transplant and heart-lung transplant program. “As ILD most commonly progresses slowly, we usually we have a few months to discuss the idea of transplantation with the patient and their family. This allows us to educate them about the pros and cons of lung transplantation and allow them to acclimate with the idea. But Joe’s case progressed very quickly, and that compressed time frame can create a lot of anxiety for patients and their families.”
That was certainly true for Paige. During the eight months of what had already been a difficult pregnancy, she undertook a daily routine that would enable her to care for her children and support Joe. In the morning, she would begin each day getting sons Finn and Brooks up and ready for the day before dropping them off with her sister or a babysitter.
She then would make the hour-long drive to Cleveland Clinic, “which is when I would get my crying done,” she says. For the rest of the day, Paige would be by Joe’s side, who was in an intensive care unit and confined to a hospital bed on high flow oxygen, a type of breathing support. Paige would leave in the early evenings and make the drive back home to put the kids to bed. Joe’s sister would alternately stay with Joe in the hospital when Paige couldn’t be there.

Paige was always by Joe’s bedside. (Courtesy: Joe Crossmon)
“It’s a bit of a blur,” says Paige, recalling that stressful time. “I was on survival mode.”
Meanwhile, Joe’s care team put the transplant process in motion. Due to the severity of his condition, and his rapid decline, Joe underwent a rapid evaluation and listing to await a compatible lung donor. As his condition worsened, Joe’s status on the waitlist increased.
After two weeks, a pair of donor organs were found. In Joe’s case, the donor’s lungs were suitable in size, blood type and immunological matching.
The surgery – complicated by Joe’s critical condition – lasted 14 hours and was performed by cardiothoracic surgeon James Yun, MD, PhD. It was successful, although Joe did experience several common complications that can occur after a lung transplant. He had minor issues with gastroparesis, a condition that causes the stomach to empty slower than normal. Doctors can treat it with medication, or in some cases like Joe’s, a minor surgery. Since the procedure, Joe hasn’t had any issues with his appetite. Additionally, he now takes insulin daily to treat diabetes caused by antirejection drugs.
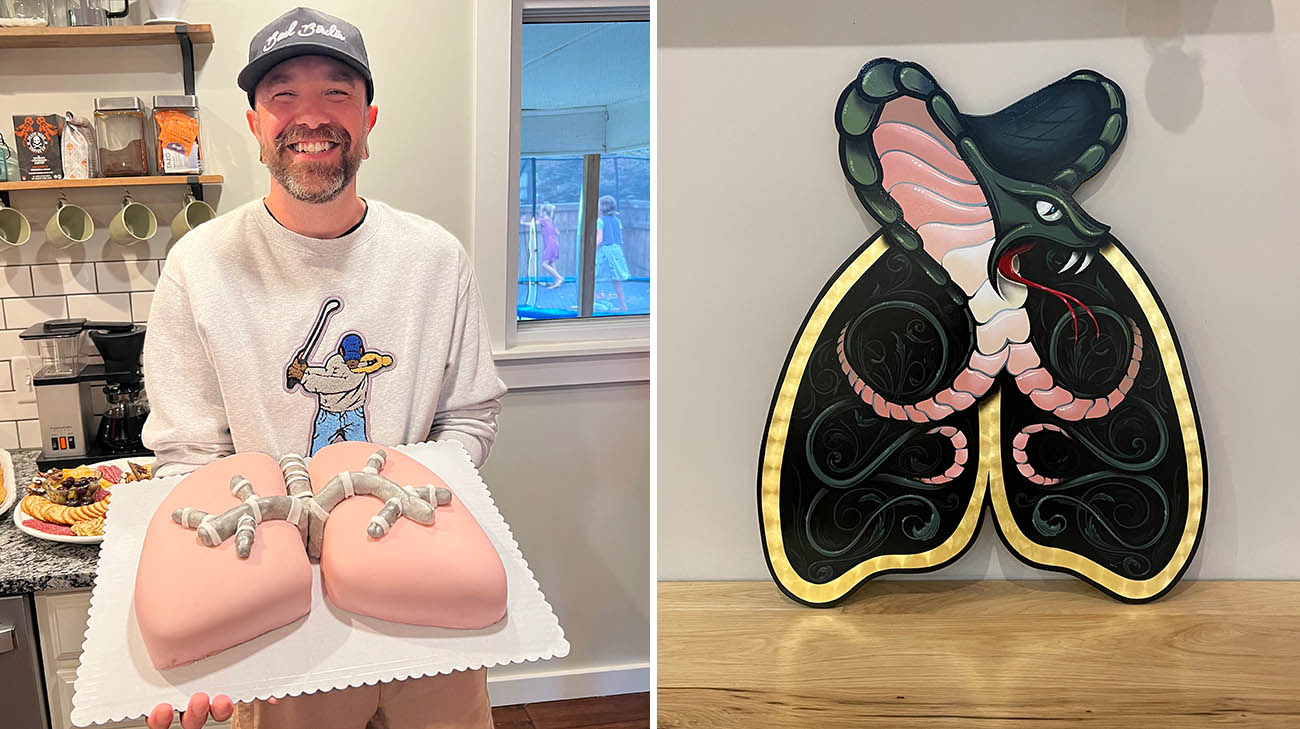
Joe is thankful to his donor and their family for the gift life. He celebrated his one year transplant anniversary with a special cake (left). Joe’s friend commissioned a hand painted piece of art for him that included a traditional cobra tattoo and set of lungs (right). (Courtesy: Joe Crossmon)
“Those are trade-offs I’ve learned to deal with,” says Joe. “But as far as the lungs themselves, and my day-to-day life, it’s all good.”
Subsequently, Joe recovered quickly and was back home on October 17, 2022. Three weeks later, Paige gave birth to their daughter. More than one year later, Joe continues to operate his tattoo business. He’s no longer tied to oxygen tanks, and he’s able to actively participate in the lives of Finn, age 5, Brooks, age 3 and 15-month-old Goldie.

Joe, Paige and their three kids, Finn, Brooks and Goldie. (Courtesy: Joe Crossmon)
“I wouldn’t have survived this without Paige,” says Joe, who expresses incredible gratitude for his donor and their family and praises the skill, commitment and kindness of the doctors, nurses and caregivers who treated him at Cleveland Clinic.
Seeing a patient thrive, and their life transformed, is exciting for the entire team, says Dr. McCurry. “A lung transplant offers a better quality and longer life. To get Joe back to where he can enjoy his life and do the things he wants to do is quite rewarding.”
Related Institutes:
Respiratory Institute,
Heart, Vascular & Thoracic Institute (Miller Family)






